Table of Contents
- What Exactly Are Bleeding Gums?
- What Causes Bleeding Gums?
- Gingivitis – The First Warning Sign
- Periodontitis – When Things Get Serious
- Brushing Too Hard
- Flossing Mishaps
- Medications That Make Things Worse
- Vitamin Deficiencies
- Hormonal Changes
- Smoking
- Stress and Its Sneaky Effects
- How to Stop Bleeding Gums: Practical Solutions
- Upgrade Your Oral Hygiene Routine
- Use an Antibacterial Mouthwash
- Try a Saltwater Rinse
- Ice It Down
- Eat for Gum Health
- Quit Smoking
- Reduce Stress
- Visit Your Dentist Regularly
- When to See a Dentist
- Final Thoughts
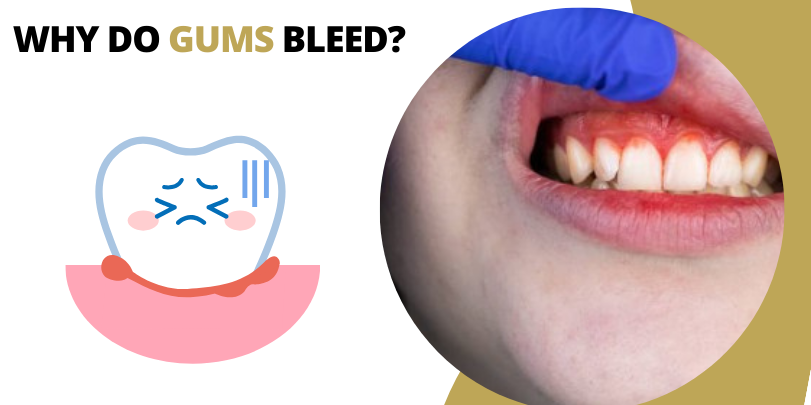
What Exactly Are Bleeding Gums?
At its core, bleeding gums refer to the presence of blood in your gum tissue, usually when you brush, floss, or even bite into something firm like an apple. Healthy gums shouldn’t bleed, so even a little pink in the sink is worth paying attention to. While a single occurrence isn’t alarming, frequent bleeding can indicate inflammation, irritation, or something more serious.
ALSO KNOW: Here’s What No One Tells You About Pyorrhea Treatment
What Causes Bleeding Gums?
There’s no single reason why gums start bleeding, often, it’s a mix of factors. Here are the most common culprits:
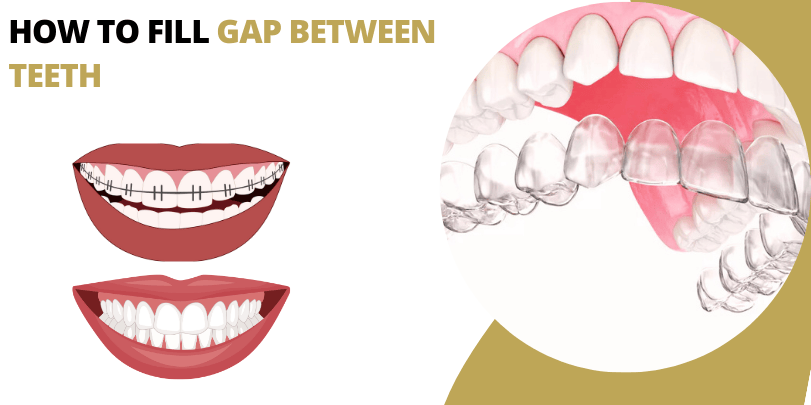
1. Gingivitis- The First Warning Sign
Gingivitis is the earliest stage of gum disease, caused by plaque buildup along the gumline. Symptoms include redness, swelling, and bleeding when brushing or flossing. The good news? It’s reversible with proper oral care. But if ignored, it can progress into something far worse- periodontitis.
2. Periodontitis- When Things Get Serious
Left untreated, gingivitis can escalate to periodontitis, a severe infection that damages the gums and can lead to tooth loss. At this stage, bleeding gums become more persistent, and bad breath, gum recession, and even loose teeth might follow.
3. Brushing Too Hard
It’s easy to think that brushing harder means cleaner teeth, but aggressive brushing can damage gum tissue and lead to bleeding. Use a soft-bristled brush and gentle, circular motions instead.
4. Flossing Mishaps
If you’re new to flossing or doing it too vigorously, you might see some bleeding. With consistent and gentle flossing, your gums should toughen up and the bleeding should subside.
5. Medications That Make Things Worse
Certain medications, like blood thinners, can make gums more prone to bleeding. If you’ve recently started a new prescription and notice more bleeding, it’s worth discussing with your doctor.
6. Vitamin Deficiencies (A.K.A. The Nutrition Connection)
Your gums need proper nutrition, too! Lack of Vitamin C (important for collagen production) and Vitamin K (which helps with blood clotting) can lead to gum bleeding. If your diet is mostly processed foods, it might be time for a nutritional upgrade.
7. Hormonal Changes (Blame It on the Hormones!)
Pregnancy, menopause, and even menstruation can make gums more sensitive due to hormonal shifts. This is why some women experience more bleeding during these periods.
8. Smoking
Tobacco use weakens the immune system and reduces blood flow to the gums, making infections more likely and healing much slower. If you smoke, your gums are at a higher risk of bleeding and overall deterioration.
9. Stress and Its Sneaky Effects
You might not associate stress with oral health, but chronic stress weakens your immune system, making it harder for your body to fight off gum infections. Plus, stress can lead to teeth grinding, which further irritates the gums.
How to Stop Bleeding Gums: Practical Solutions
Now that we know what causes it, let’s talk about what you can do to stop the bleeding and keep your gums healthy:
1. Upgrade Your Oral Hygiene Routine
Switch to a soft-bristled toothbrush. Hard bristles can be too harsh. A soft-bristled brush cleans just as effectively without damaging the gums.
2. Use an Antibacterial Mouthwash
A good mouthwash can help kill bacteria that contribute to gum inflammation.
3. Try a Saltwater Rinse
Saltwater rinses can soothe inflammation and reduce bacteria. Mix half a teaspoon of salt in a glass of warm water and swish for about 30 seconds.
4. Ice It Down
If your gums are swollen and bleeding, applying a cold compress to the outside of your cheek can help reduce inflammation and slow the bleeding.
5. Eat for Gum Health
Load Up on Vitamin C – Citrus fruits, bell peppers, and leafy greens help strengthen gum tissue.
Increase Your Vitamin K Intake – Found in spinach, kale, and broccoli, it helps with blood clotting.
Stay Hydrated – Water helps wash away bacteria and food particles.
6. Quit Smoking
This one is a game-changer. If you smoke, cutting back or quitting altogether can drastically improve your gum health.
7. Reduce Stress
Incorporate stress-relief activities like exercise, meditation, or deep breathing to keep your immune system strong and your gums resilient.
8. Visit Your Dentist Regularly
If your gums bleed frequently, don’t wait until it’s too late. A professional cleaning can remove plaque and tartar buildup that brushing alone can’t tackle.
When to See a Dentist
If bleeding gums persist for more than a week despite improving your oral hygiene, it’s time for a professional check-up. Seek immediate dental care if you notice:
- Gums that are constantly swollen or painful
- Bad breath that won’t go away
- Receding gums
- Loose teeth or pus around the gums
These could indicate advanced gum disease or another underlying health issue that requires treatment.
Final Thoughts
Bleeding gums may start as a minor issue, but if left unchecked, they can lead to serious dental and even systemic health problems.
By maintaining good oral hygiene, eating the right nutrients, managing stress, and seeing your dentist regularly, you can ensure that your gums stay strong, healthy, and free from bleeding.
A little care today can save you from major dental woes tomorrow. So, next time you see a bit of red in the sink, don’t ignore it, your gums are trying to tell you something!
Written by DR. PUNEET KATHURIA B.D.S., M.D.S., F.I.C.O.I. (USA)
 Australia No
Australia No Canada No
Canada No India Toll Free No
India Toll Free No UK No
UK No USA No
USA No